Osteoporosis is the most common metabolic bone disease that I see in practise. It is characterised by decreased bone density and an increased risk of fracture. Osteoporosis is usually overlooked and undertreated because it is clinically silent until it presents itself as a fracture. This can cause devastating physical and psychological effects on a patient.
Osteoporosis significantly increases the risk of fractures at the proximal femur, the distal end of radius, the proximal humerus and vertebral body. The World Health Organization’s standards for diagnosing osteoporosis use dual-energy x-ray absorptiometry (DEXA) to measure bone mass density.
Osteoporotic Vertebral Compression Fracture (OVCF)
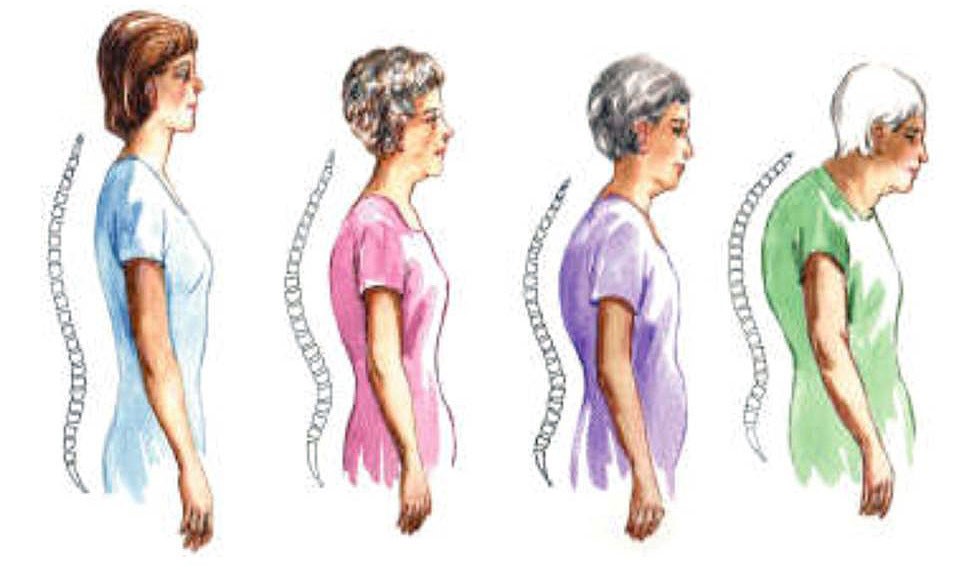
OVFC is the most common complication of osteoporosis, especially in postmenopausal women. Two third of the patients remain pain-free. A single compression vertebral fracture, however, is associated with a measurable loss of height. Patients with progressive hunching of the back or loss of height (Fig 2) may suggest OVCF and should be evaluated for this complication.
One third of OVCF is painful, and usually associated with very minor trauma or simple movements such as bending forward, vigorous coughing or sneezing. The majority of painful OVCFs resolve in three to six weeks, but a small number of patients will face severe pain or even neurological deficits.
Painful OVCF
This occurs when patients have severe mechanical pain and refuse to move or get out of bed. If this is not treated properly it can lead to severe debilitating complications such as:
- Prolonged immobilisation
- Worsening of osteoporosis
- Depression
- Poor oral intake
- Poor effort tolerance
All these complications can lead to further deterioration of the patient’s general health.
Investigation
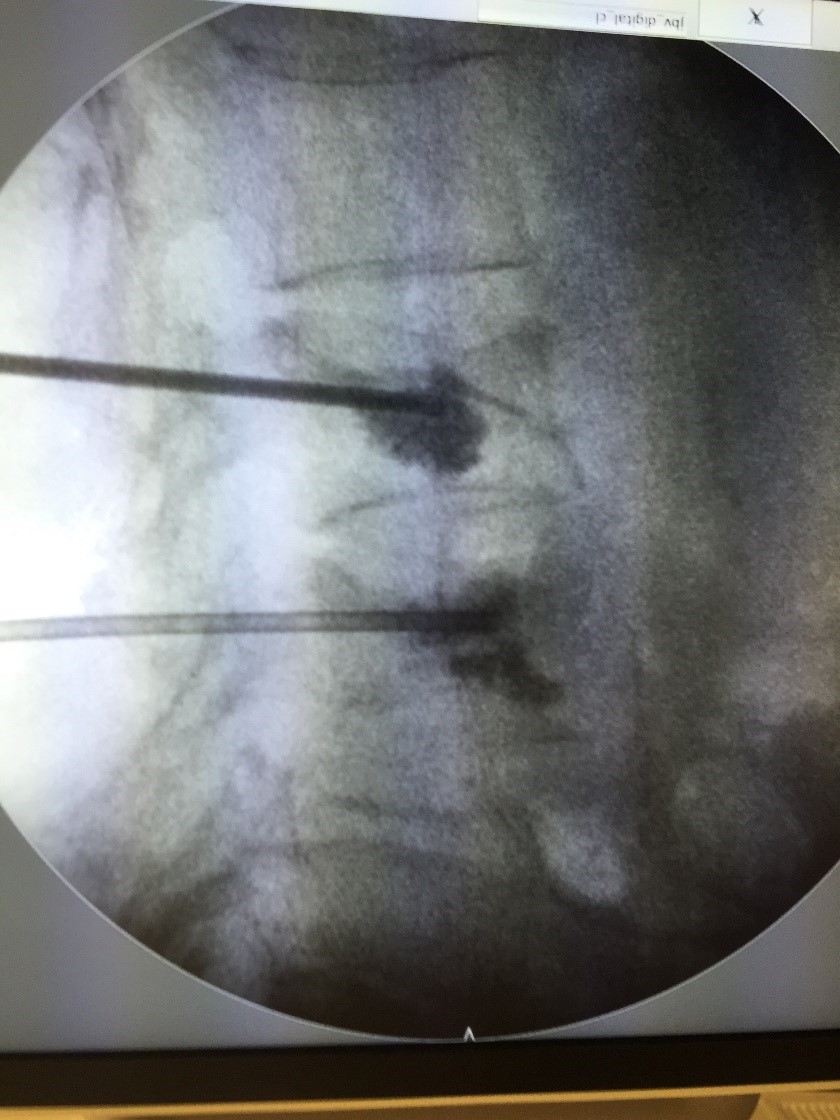
Vertebral compressions can be confirmed with an X-ray (Fig 3) or Magnetic Resonance Imaging (Fig 4).
Treatment
Medication
All patients should be treated with elemental calcium with vitamin D and anti-osteoporotic drugs recommended by the treating doctor. Pain medication such as paracetamol or nonsteroidal anti-inflammatory drugs (NSAIDs) should be given to alleviate pain. Narcotic medications may be necessary for patients with severe pain who do not respond to normal painkillers.
Bracing
A hyperextension brace (Fig 5) has been shown to be helpful in treating painful vertebral compression fractures. It helps to prevent further collapse of the vertebral and reduces pain.
Exercise
Once pain is reduced or ended, patients should begin exercises that enhance the axial muscle. Back extension exercises are preferable to abdominal flexion exercises that may further collapse the flattened vertebral.
Surgical intervention
Although most patients recover from the acute pain of new vertebral compression fractures within three to six weeks, a minority of patients continue to experience persistent mechanical back pain. These patients may be candidates for surgical intervention.
Percutaneous Vertebroplasty and Kyphoplasty
Vertebroplasty and kyphoplasty (Fig 6) are minimally invasive procedures designed to relieve pain by injecting medical cement into the fractured vertebral. Hardening of the cement provides immediate stability and pain relief.
Open Surgery
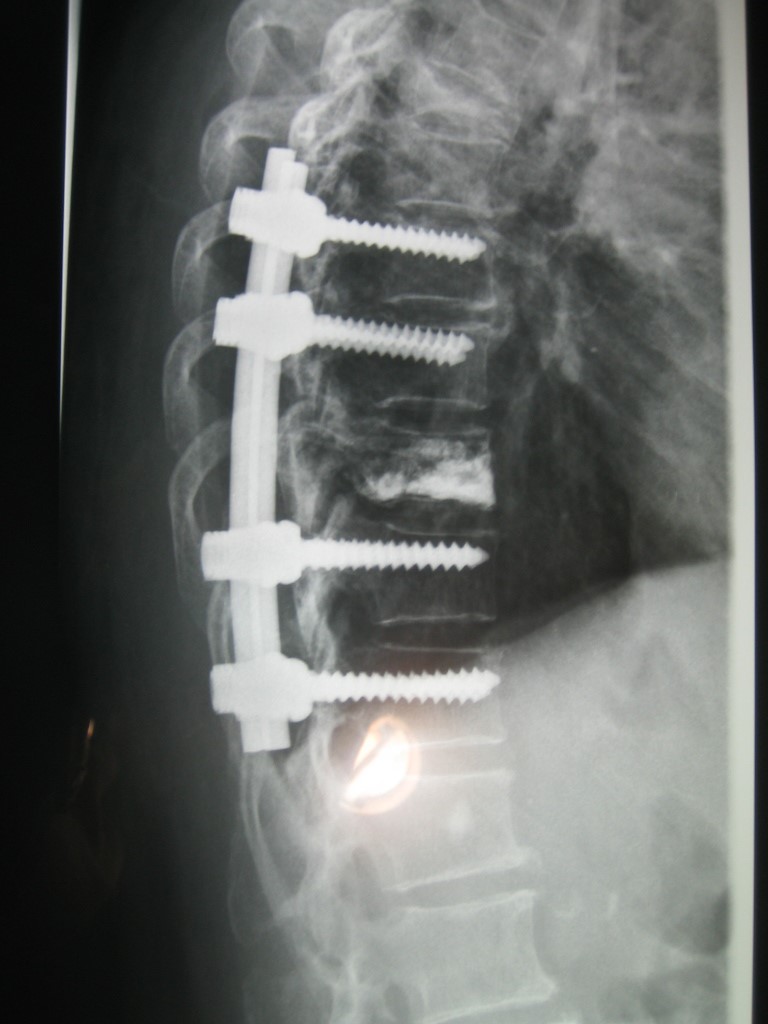
Open surgery (Fig 7) is rarely necessary and has severe complications due to the osteoporotic bone quality. Indications for open spinal surgery are:
- OVCF with neural compression that requires surgical decompression of the involved neural tissue
- Painful OVCF with excessive or progressive kyphosis
- Painful OVCF with excessive collapse where vertebroplasty is not feasible
Open spinal surgery involves decompression of the neural tissue and stabilisation of the spine using a pedicle screw, which provides a means of gripping a spinal segment.
Pain today, gone tomorrow
Most OVCF is asymptomatic, but one third presents pain. The pain can be treated with analgesics, resulting in the majority of cases becoming pain-free in three to six weeks. A small number of patients, however, face persistent pain after six weeks. This can be treated with percutaneous vertebroplasty and kyphoplasty. Open spinal surgery should be the last treatment option due to its high complication rates.