Psoriatic Arthritis (PsA) is basically a type of inflammatory arthritis which is closely associated with Psoriasis (PsO). Psoriasis is a skin condition whereby one can get scaly red and white patches mainly over the scalp, elbows and knees. However generally PsA only affects people with psoriasis in 20% of cases and if so tends to develop within 10 years of first having been diagnosed with psoriasis. What causes PSA/PsO is not known exactly. About 40% of patients have an affected family member. It can also be affected by an infection that activates the immune system.
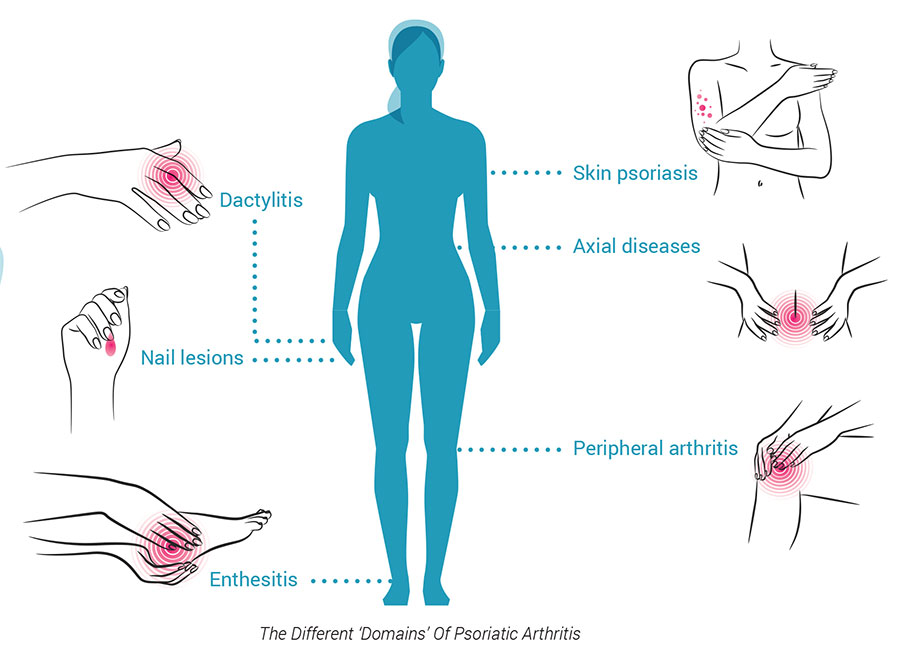
PsA and PsO are both autoimmune conditions in which the body’s immune system goes into overdrive and attacks the body. Psoriatic symptoms can flare and subside, vary from person to person and even locations in the same person over time. It can affect any joint in the body, it can affect just one joint, several joints or multiple joints. Generally, affected joints can resemble a swollen sausage, a condition referred to as dactylitis. Finger and toe nails can also be affected.
It typically affects people in middle age but can affect at any age. PsA in the spine is called spondylitis, it causes stiffness in the back or neck and limited range of movements of the spine. PsA can cause tender areas/spots at areas where tendons and ligaments inserts onto the bones ie enthesitis and this is a characteristic feature.
To diagnose psoriatic arthritis, a rheumatologist would look for swollen and painful joints, patterns of joints involved and skin and nail changes typical of psoriasis. Blood tests are done to rule out other types of arthritis and make a definitive diagnosis. Blood investigations may reveal high levels of inflammation (ESR/CRP levels) and mild anemia. Occasionally skin biopsies are needed to confirm a diagnosis. X-rays, joint ultrasound and MRI help look at the joints in more detail.
There a few patterns of PsA. It does not really affect a single joint pattern such as one would see in osteoarthritis or rheumatoid arthritis. Common recognized patterns include symmetrical polyarthritis like rheumatoid arthritis and is more common in women and affects commonly the hand joints. Another pattern is known as asymmetrical pauci-arthritis whereby it only affects a few joints and this pattern tends to affect of a few of the digits of the fingers and toes. The final big group is the spondylitic pattern whereby there is associated back stiffness, sacro-ilitis and atlanto-axial (neck joints) joint involvement. Other areas are the spine, archilles tendon and the plantar fascia.
On examining a patient, special attention is given to the skin ie plaques of psoriasis. Pitting of the nails ie tiny pits can be seen on the nails. Also seen on the nails is onycholysis which is a separation of the nail from the nail bed. Other signs include arthritis, dactylitis and enthesitis. Other associations with PsA is eye disease ie conjunctivitis and uveitis, and aortitis which is inflammation of the aorta which is the large blood vessel in the body.
Any patient with a diagnosis of psoriasis should be screened for arthritis every year. If there is presence of joint pains, dactylitis or enthesitis they should be referred to a rheumatologist.
Treating PsA varies depending on the patients level of pain, swelling and stiffness. Anti-inflammatory medication, disease modifying anti-rheumatic drugs and sometimes a combination of these drugs are used. There are also several biologic type medications available to treat via infusion or injections.
The broader impact of PsA depends on the joint involved and the severity of symptoms. Fatigue, mood changes, depression and anemia are common. Treating the pains and reducing the inflammation generally helps. People with PsA and PsO are slightly more likely to develop high blood pressure, high cholesterol, Type 2 DM and obesity. Hence treating these factors are an important aspect of treatment.
Most people develop some joint stiffness and weakness due to lack of use, hence proper exercise is important for overall health and to keep the joints flexible. Swimming, cycling and walking are excellent types of exercise recommended for arthritis generally.
A rheumatologist will be the best to make a proper diagnosis, assess the disease and advise about the best treatment options.